They’d always checked temperatures inside this house. Twice a day the thermometer was moved from bedroom to bedroom, tucked under five arms, offering five beeps and five numbers, assurances that the women who lived here were, for now, okay.
A beep for Andrea Outman, whose oxygen tubes curved around her wheelchair, the only resident of the house who could fully communicate through speech. For Carolyn Davis, the only one who could walk, her graying braids bouncing as she paced. For Ericka Yates, who kept being taken back to the hospital, the complications of her medical history complicating her life again.
A beep for Wah Der Yee, who had spent nearly her entire life in a Virginia-run institution before moving to this suburban ranch in Dumfries, one of America’s more than 76,000 group homes for adults and children with disabilities. Here, medical care was mixed with dance parties and craft classes, grocery runs and dinner outings, neighborhood walks and park picnics. Or it was, until the coronavirus pandemic hit.
By that Tuesday in May, the women had spent 56 days inside their Northern Virginia home, as their caregivers tried to keep the coronavirus out. Now it was Day 57, and the fifth resident, whose guardian asked that she not be named, was getting her vital signs checked. Blood pressure, oxygen level and then, the beep of the thermometer.
‘This is clean now’
Before the wipes were opened, they were wrapped in plastic film and marked with a serial code, a number that tracked their entire journey. To follow the wipes is to watch the pandemic unfold in slow motion, making its way to all the places the canisters, and the crisis, would eventually go: airports trying to reassure travelers, day cares teetering on bankruptcy, parking lots turning into testing sites.
The wipes that wound up at the Virginia group home were manufactured on Dec. 30, 2019, the same day authorities in Wuhan, China, first warned local hospitals of a “pneumonia of an unknown cause.”
Inside a Midwestern factory, rolls of a material made of microscopic plastic fibers and wood pulp were stuffed into canisters and squirted with cleaning liquid and fragrance, at a rate of several hundred every minute.
Add a lid and a label, and the result is a product whose purpose is the same as hundreds of other disinfecting products. And yet, the convenience of eliminating messes and “99.9 percent of germs” with one simple swipe, the satisfaction of disappearing those problems into the trash, has proved irresistible to American shoppers since Clorox, Lysol and Mr. Clean all debuted disinfecting wipes two decades ago.
As the group home’s canisters were leaving the factory, the World Health Organization was investigating the mysterious illness that had sickened at least 27 people in China. By the time the first coronavirus case was confirmed in the United States three weeks later, the canisters had already passed through two warehouses in Illinois and Maryland.
As they arrived at Schenck Foods, a distributor in Northern Virginia, on Feb. 12, much of the world was coming to understand that it was in the midst of a mess that could not be so easily wiped away. Clorox started running its manufacturing plants 24 hours a day. The company had been bracing its shareholders for a mediocre year. Instead, in sales, stock price and surveys of whom Americans trust, Clorox would become one of the pandemic’s biggest winners, and wipes its most coveted trophy.
On March 6, 240 of those canisters were loaded into a box truck, along with $1,945 worth of disinfecting spray, hand soap and jugs of bleach, all bound for the Arc of Greater Prince William County. President Trump was a week away from declaring a national emergency. But at the nonprofit, Donna Shipman was already preparing for chaos.
Before she became a supervisor, Donna had worked as a direct support professional like Angela. She understood that to someone with intellectual disabilities, even the slightest change in routine could feel like their world had imploded.
Soon, every day would bring the cancellation of something the nonprofit’s 2,200 clients depended on. Then came weeks of comforting caregivers who’d been kicked and bitten by group home residents in distress, calming parents who’d been barred from visiting their children, apologizing to staff members they couldn’t afford to keep.
By the time Clorox was warning Americans not to ingest bleach as Trump had suggested, disabled communities were battling outbreaks. At a state-run facility in Illinois where half of the 336 residents are nonverbal, 237 of them and 160 of their caregivers had tested positive by mid-November. Four employees and seven residents there have died.
Though large facilities like it still exist in at least 36 states, decades of abuse allegations, lawsuits, court decisions and Justice Department interventions have whittled away at their numbers. In Virginia, just one remains. The Trump administration has refused to track outbreaks at such institutions or in group homes, meaning there is no national count of how many people with disabilities have become infected or died of the virus.
But on May 13, the Virginia group home learned its fifth resident had indeed tested positive. Donna unlocked the closet where she’d stashed the Clorox wipes and other supplies and carried them to her car. Unaware that she, too, would soon be showing symptoms, she delivered the wipes to their final destination.
She could see the anxiety in the caregivers, who in the days ahead were going to be exposed again and again. They knew they could not stop the virus from spreading through the air. But she hoped the canisters would, in some small way, ease their fears about surfaces.
“I wanted to give them a sense of comfort,” Donna said. “They can wipe the wheelchairs, the tables, the doorknobs, anything, and know, okay, this is clean now.”
With no specialized access to testing, the staff drove Andrea, Carolyn, Ericka and Wah to their doctors to have their nostrils swabbed.
The caregivers were told to find their own way of getting tested. Angela, who’d had the most contact with the sick resident, opted for a drive-through testing site in a Walmart parking lot. She rolled down her window, administered her own swab and returned to work.


*Ericka Yates, 44, had to be quarantined in her room when another resident of her group home contracted the coronavirus. (Amanda Voisard for The Washington Post)*
‘How many more days?’
Angela had a routine so boisterous, she sometimes annoyed the other caregivers. At 6 a.m., she’d start her shift in the room where Wah and the fifth resident slept under the watchful eyes of their stuffed animals. She’d flip on the radio and sing along, even when she didn’t know the words.
Wah, a 56-year-old whose tongue was permanently protruding, rarely made noise of any kind. But for Angela, she would let out long, guttural wails, almost as if she was singing along.
Since Wah had left the Northern Virginia Training Center, where she’d lived since age 5, her caregivers had marveled at all the little changes that, for her, were big. Rather than stare in the same direction all day, Wah began turning toward people she wanted to see and away when she wanted to be left alone. Though her fingers rarely moved, she started to wave her arms. With specialized shoes made for her uneven legs, she used a supportive box to stand, her head bobbing to the classical music they played for her. But no one could get Wah to interact quite like Angela, for whom she would even lift her arms as she slid into a new shirt.
That was Angela’s job: knowing what each resident needed to be fully herself. That Ericka, 44, would stop crying mid-meltdown if she could watch paper be shredded. That Carolyn, 62, loved to hold her hand and take her on a tour of the house’s lightbulbs, which Angela would switch on and off. That Andrea, 37, preferred “Dora the Explorer” to “Bob the Builder.”
“I used to live with my parents, but I changed to the group home because Mom can’t take care of me,” Andrea explained. Her parents, now in their 70s, spent the first two years of her life visiting their premature daughter at Children’s National Hospital, where she breathed through a tube coming out of her neck. For decades they navigated surgeries and scares and doctors’ prognoses that Andrea wouldn’t survive another year, until they began to worry that it was they who wouldn’t be around much longer. They placed Andrea on Virginia’s wait list for services, which currently numbers 13,000 people. Nineteen years passed before a spot opened up in a house for the “medically complex,” where Andrea would have no one to talk to but the people who cared for her.
At the Dumfries group home, they understood that Andrea could have the cognitive level of a 5- to 7- year-old and still be a grown woman. Angela drove Andrea to her parents’ house for visits, treated her to Dunkin’ Donuts after her doctor’s appointments and chaperoned her Applebee’s dates with Mark, who lived at another group home. The pair had once exchanged rings at an unofficial wedding ceremony orchestrated by the staff.
“Did you know I got married to Mark?” Andrea said. “It feels nice to be married. As much as we bicker, we still love each other.”


*Andrea Outman, 37, brushes her teeth while Margaret Acheampong helps her get ready for bed. (Amanda Voisard for The Washington Post)*




*Andrea spent the first two years of her life in a hospital, and her parents have been told multiple times throughout her life that she wouldn\’t survive much longer. She is now 37. (Family photo)*
But now, Andrea wasn’t allowed to leave her room. She could hear Ericka crying across the hall. Carolyn couldn’t walk around the house. Wah was stuck in the living room. They had all tested negative for the coronavirus, and by Sunday, their 62nd day in the house and their fourth in a house with covid-19, their vital signs showed that so far, they seemed to be okay.
Every time the staff checked on the sick resident, who wasn’t showing any more symptoms, they wore gloves, a gown or trash bag, shoe coverings, a face shield and a KN95.
Angela, who still hadn’t received her test results, wiped every surface, checked on the other residents, then wiped again.
“How many more days?” asked Andrea, tired of cutting up magazines to pass the time.
The next day, she asked again. But Angela wasn’t there to answer her. She didn’t come back the next day, either. No one had to explain to Andrea what that meant.


‘What’s incubation?’
The test results came back negative, but Angela felt as if she’d been Velcroed to her couch whenever she wasn’t hunched over in the bathroom. Her sister poured her a can of chicken soup, and knew just how sick Angela was when she returned the next day to find the half-empty bowl still sitting out.
At another time, Angela would have acted as if disregarding a dish was an insult to her moral code. She ranted about co-workers who didn’t keep the group house or its residents impeccably clean. If she discovered another caregiver had left a resident soiled for too long, Angela would call her son Merritt and ask, “Can you believe this motherf—-r?”
What Merritt couldn’t believe, at first, was the tenderness his mother showered on the people she cared for, so different from the tough-love approach she’d taken with him. Angela had become a mother at 15 and raised Merritt on her own. After working at her mom’s soul food restaurant, Ann’s Wings and Things in Stafford, and at an insurance company, Angela was 50 when she signed up for a two-week course to become a direct support professional. Soon she was calling the residents “my individuals,” frying fish for them on her days off and wheeling them into her own family’s gatherings.
“When she was working, it was like, I never knew she had that love in her,” said Merritt, now 47. “It was unreal, her care for them. It almost made me a little bit jealous.”
For all the messes cleaned and meals cooked, Angela’s starting salary was $11 an hour. More than half of direct support professionals quit within a year, with 88 percent citing inadequate pay as a reason for leaving in a recent national survey. But Angela kept at it for more than a decade. Her son lived with her and helped pay her mortgage.
Tension over money gnawed at their relationship for years, until, after one of their biggest fights about who was paying for what, they stopped talking. He moved out. Their relatives thought it would pass.
But three years later, Merritt’s Aunt Bertha was the one to phone him with news. “Your mom’s really not feeling good,” she said. “You need to call her.”
A week after the symptoms started for Angela, Bertha Johnson drove her back to Sentara Hospital. She had to use a wheelchair to get her inside. She made sure Angela’s bosses knew she wouldn’t be back at work. By then, another caregiver from the house had tested positive. So had Donna, who’d delivered the Clorox Wipes.
And hours after Angela was admitted to the hospital, she learned that her first test was wrong. She had tested positive, too.
This disease was devastating Black families like hers. But Angela had no intention of becoming another statistic. She didn’t have underlying conditions. She walked her pit bull Raven miles every day. She was strong enough to lift 200-pound residents.
“Please call me,” her sister texted, a week into her hospital stay. “I am really worried. You know I already have a ton of gray hair. Don’t need any more.”


*Angela\’s sister Bertha Johnson and son, Merritt Johnson, couldn\’t visit her in the hospital. (Amanda Voisard for The Washington Post)*
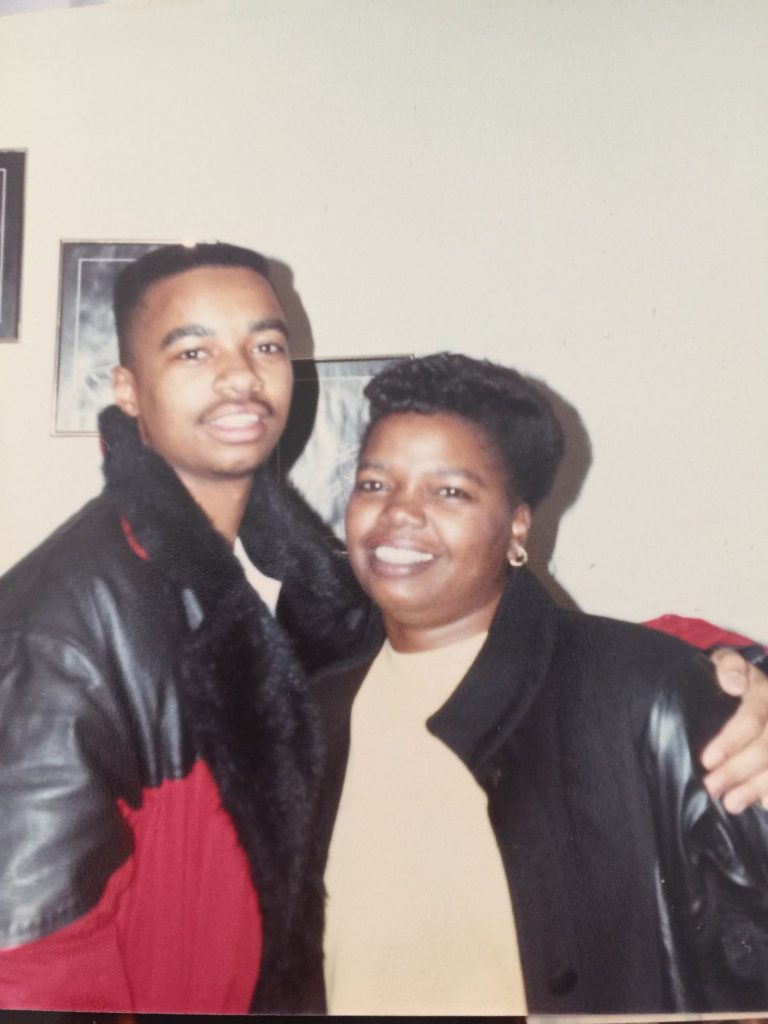
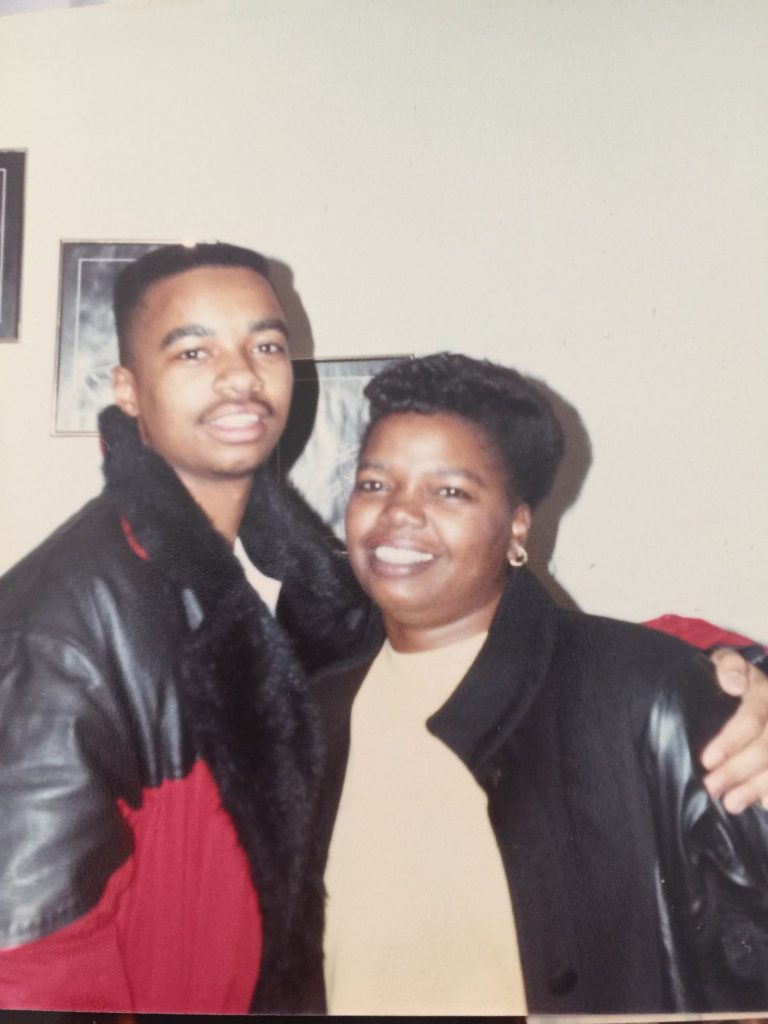


*Top: Angela with her son when he was a teenager. (Family photo) Bottom: Angela kept a photo of herself with her sister on her refrigerator. (Amanda Voisard for The Washington Post)*
“Girl, I look so good,” Angela told her, two weeks in. “My legs are so skinny!”
“I talked to Merritt,” Angela revealed on Week 3, after her son called and told her, “When you get out of there, we are going to make up for all the lost time. We shouldn’t have went this long.” He thought her voice sounded slow and slurred as she asked him, “Do you mean it?”
He called again on June 21, to tell his mother, as he once did every year, “Happy Father’s Day.” To him, she’d always been both.
“What’s incubation?” Angela asked her sister two days later. Bertha didn’t know, but said she would research it. When she called Angela’s hospital room the next day, to tell her the word was intubation, another patient answered the phone. Angela had been moved to the ICU.


*In her last hours, Angela\’s sisters were able to visit her in the hospital and take this photo of her through a glass window. (Family photo)*
Only at the very end did the hospital allow Bertha and her sister Dorothy to come see Angela, and only through a glass window. There she was, the woman who cared for people who couldn’t care for themselves, with tubes running down her airways, her chest puffed up from a ventilator, unable to speak, unable to understand.
Bertha stood listening to a machine’s beeps grow further apart. She watched the little digital number go down.
Angela’s heart rate was slowing, and slowing, and then, it was stopped.
‘Deserve that respect’
“Every year, they tell us how much they support us,” a woman on the Zoom call declared, her face slightly pixelated. Donna Shipman leaned onto her desk, trying to listen. The covid-19 symptoms she’d developed after delivering the Clorox wipes to the group house had kept her out of work for almost two months.
She didn’t know for sure where she’d gotten infected, but she knew she’d passed the virus to her 11-year-old daughter. The girl had no sense of taste for weeks, and after recovering, became so nervous about getting infected again that she had to see a therapist. Now Donna was back at the nonprofit, begging the state’s lawmakers for more support at a virtual rally in early October.


*Donna Shipman, right, and her 11-year-old daughter Madison. (Family photo)*
Kim Goodloe, board president of the Arc of Virginia, was on her screen, talking to the handful of legislators who’d logged in.
“They tell us how much they really want to do for us,” Goodloe continued, “And what do they do? They do 1 percent.”
One percent: the cut of the $3.1 billion in Cares Act funding that Virginia initially gave to programs for people with intellectual and developmental disabilities. The state’s nursing homes were receiving an extra $20 per resident, per day. Group homes spending hundreds of thousands on staff overtime got nothing. Disability advocates pressuring Congress for more support had little success too.
Donna turned off her mute button and took a deep breath, her lungs still not filling the way they should.


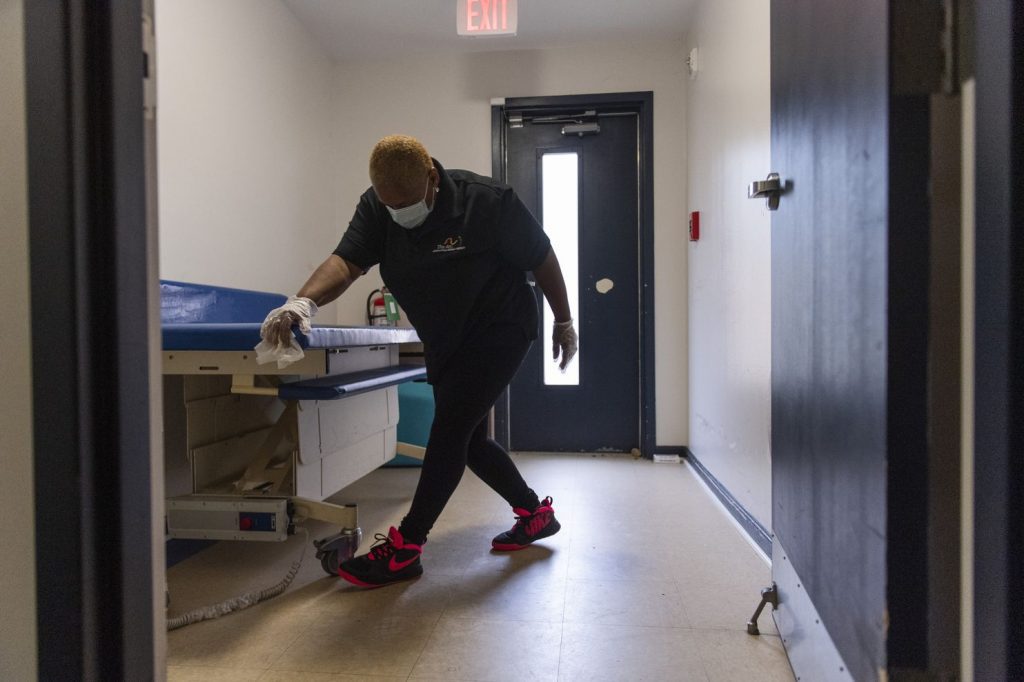
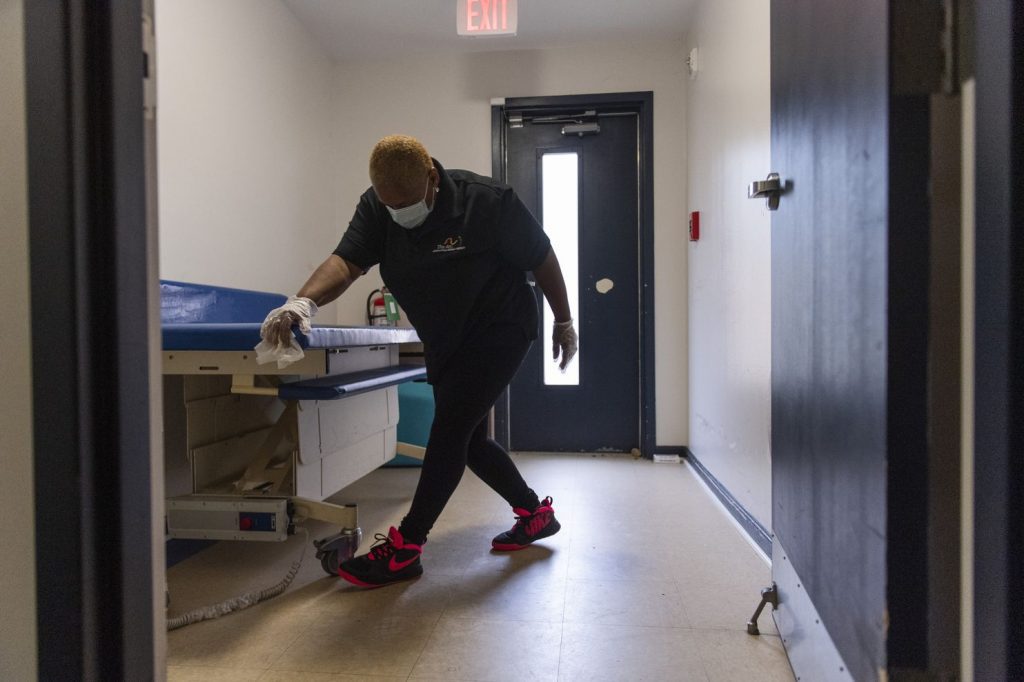
*Faustina Baiden, a direct support professional, cleans after helping Andrea get in bed. (Amanda Voisard for The Washington Post)*
“We watch the news every day and we see the acknowledgment and the respect, consideration and funding that is given to hospitals, nursing homes and assisted-living facilities,” she told the lawmakers. “I do not ever want to slight them because they are our health provider brethren. But we also deserve that respect.”
A few weeks later, disability service providers that run group homes and other programs in Virginia were told they would receive increases in Medicaid payments that the pandemic had halted. Gov. Ralph Northam (D) announced $1,500 bonuses for 43,500 home health workers, who care for the elderly and others in private homes, in appreciation of the risks they have taken. But direct support professionals in group homes wouldn’t be included.
A local grant made it easier for Donna to buy more protective equipment and supplies, but she hadn’t been able to order any more Clorox wipes. Her supplier could never restock them. Grocery stores limited how many canisters customers could buy.
Clorox had hoped that by contracting with 10 additional manufacturers, there would be enough wipes by late summer. It wasn’t enough. By fall, the company predicted it could not meet the demand for wipes until 2021, even though it was shipping nearly 1 million packages of wipes per day.
Companies were using the presence of wipes to give employees confidence to return to work. Teachers were being told to disinfect entire classrooms every hour. Sitting beside Amy Coney Barrett at the hearings for her Supreme Court nomination was an industrial-sized canister of Clorox Disinfecting Wipes, Fresh Scent.
But at the group home where Angela once worked, the caregivers had long since returned to killing germs with spray and paper towels.


*Andrea waves to Idmatu Ayoub, a nurse who looks after her at the Arc of Greater Prince William day program. (Amanda Voisard for The Washington Post)*
‘We loved each other’
The hum of Andrea’s oxygen machine was the only sound in the early morning darkness. She’d never gotten sick, and neither had her housemates. The fifth resident’s fever went away after a week. Charles Traore, the other caregiver who became infected but recovered, was now the one to wake the women up each day.
He didn’t flip on the radio. There was no singing. He helped them into their clothes, fed them breakfast and on this day in October, rolled them down a ramp in the garage. After 203 days in the house, they finally had somewhere to go.
With ponchos draped over their wheels, they were lifted into the transport van for a 20-minute ride. Then a caregiver boarded the bus with a thermometer. Four beeps later, they were guided into the Arc’s day program, which had decided that Andrea, Carolyn, Ericka and Wah could try to return, slowly, to the life they once recognized.
Another staff member’s positive test would send them back home in a few weeks. But for now, they could spend the day in a bleach-scented classroom with crafts taped to every wall. Carolyn reached for her caregiver’s hands, asking to go for a walk. Ericka, seemingly confused at the change in scenery, cried for two hours, as Andrea raised her voice to be heard over the noise.
“I’m going to keep coming back here?” she asked. “Tomorrow, too?”
“Yeah, we’re going to keep coming back,” the day program director told her. “Or, until we tell you not to, how about that?”




*Before entering their day program, Carolyn and the other residents had to have their temperatures checked. Inside, physical therapist Sherry Mielnicki helps them exercise by dancing. (Amanda Voisard for The Washington Post)*
No one had told Andrea about Angela’s death. Her parents had asked the staff not to, wanting to explain themselves. But by the time they tried, Andrea already knew; she had seen the other caregivers crying.
“She would take me everywhere, but now I can’t go because there is no one to take me except Charles, but he won’t do it because I have to be in here,” Andrea said, reaching for a “Paw Patrol” DVD. “We loved each other. Oh God, I don’t want to talk about it. I don’t. I don’t.”
Wah sat with her hands clamped in her lap. No one had told her about Angela, either.
They said nothing because they believed that somehow, even before Angela’s sister texted the news, the always quiet Wah already knew her favorite caregiver was gone. For hours that day, her long, loud wails filled the house.
Now, she was silent again. People at the day program came to greet her through their masks. She turned her head away.


*Wah is lifted into her bed inside the group home. (Amanda Voisard for The Washington Post)*


